This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Gynaecology
Gynaecology
Contraceptive methods
Modern women choose to use contraception for a variety of reasons, including:
- Controlling and avoiding an unwanted pregnancy
- Protection from sexually transmitted diseases (condom)
- The benefits that contraceptive pills provide, in addition to contraception
Globally, it is estimated that 63% of women of reproductive age (77% in the US) who are in a relationship use some form of contraception. Despite this, the rate of unwanted pregnancies remains high, with a significant impact on women’s physical and mental health. It is estimated that this rate in the US is 5%, which translates into 3.2 million unintended pregnancies per year.
No contraceptive method is perfect, each one has its advantages and disadvantages, its medical indications and contraindications and should be adapted according to the woman’s needs and requirements by the attending gynecologist.
Thus, enumerating the various contraceptive methods we distinguish:
- The condom (male or female)
- Spermicides
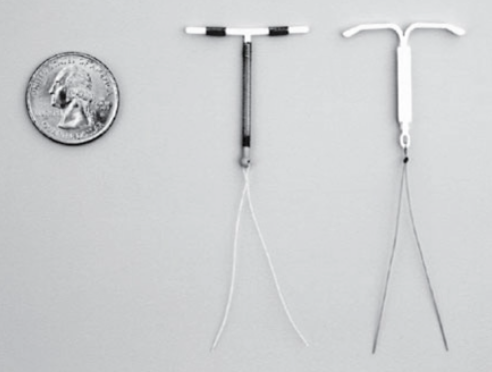
- The various spirals
- The pill
- Intravaginal rings
- Dermal patches (patches), subcutaneous inserts
- Surgical ligation of the fallopian tubes in women
- The surgical ligation of spermatic ducts in men
- Intermittent intercourse
- Emergency contraception (morning after pill)
The effectiveness of each method is evaluated worldwide using the Pearl index, which is defined as the number of unwanted pregnancies per 100 women per year (or the number of pregnancies in 1200 months of contraceptive method use).
Consequently, the smaller this number, the more effective the contraceptive method.
So, according to decreasing efficiency, based on this indicator we distinguish:
- Subcutaneous inserts 0.05% PI (Pearl Index)
- Ligation of spermatic ducts in men 0.15% PI
- Hormonal coil (spiral) 0.2% PI
- Tubal ligation in women 0.5% PI
- Coils with copper 0.8% PI
- Injectable hormonal contraception 6% PI
- Pill 9% PI
- Dermal patch (pat) 9% PI
- Intravaginal ring 9% PI
- Diaphragm 12% PI
- Male condom 18% PI
- Female condom 21% PI
- Intermittent intercourse 22% PI
- Abstinence during fertile days 24% PI
- Spermicides 28% PI
Hormonal methods of contraception provide other benefits to the woman.
More specifically, the birth control pill
- reduces period pains
- reduces pelvic pains associated with endometriosis
- reduces blood loss during the period, thus improving the hematocrit (in case of iron deficiency anemia)
- reduces the possibility of ectopic pregnancy
- reduces the symptoms of premenstrual syndrome
- reduces the possibility of benign breast pathology
- reduces the risk of ovarian cancer
- reduces the risk of endometrial cancer
- reduces the risk of colon cancer
- reduces acne problems
- reduces hair growth
- regulates the cycle
Hormonal contraception, in addition to its most well-known and widespread form, which is the pill, can also be administered in quarterly injectable form, in the form of a subcutaneous insert, lasting three years, in the form of a monthly intravaginal ring, skin patch (patch) or even endometrial rings.
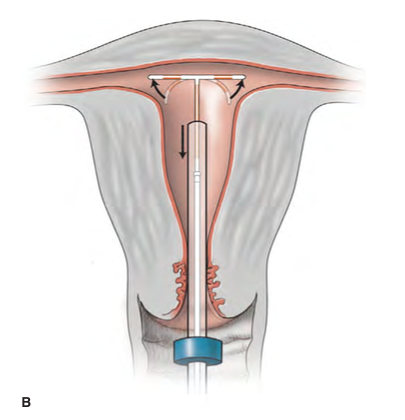
The placement of an endometrial coil (spiral) can be done in the doctor’s office without anesthesia or in the hospital (short-term anesthesia). It is usually preferred in women who have already given birth, while the duration of effectiveness is 3-5 years depending on the type.
Also, regardless of the duration of use, fertility returns to age-normal levels after stopping contraception when the woman decides to do so.
One thing that should be understood is that these forms of contraception do not provide protection against any sexually transmitted disease, which is only achieved with a condom.
As far as contraindications are concerned, these should be recognized by the attending gynecologist and the appropriate form of contraception adjusted accordingly. In general, hormonal contraception is contraindicated in a history of breast cancer, in known thrombophilias, in a history of thrombosis, etc., while non-hormonal methods (e.g. IUDs) are contraindicated in anatomical abnormalities of the genital system. In most cases, however, there are alternative solutions, so the most suitable one is also adapted.
But at what age can a woman safely stop using her contraception?
The average age of menopause is 51 years. If the woman is using hormonal contraception, then a good approach is to switch to another form of non-hormonal contraception and continue it for up to a year after the end of the last period. If the woman is already using a non-hormonal type of contraception and is older than 50 years, then she maintains it up to one year after the end of the last period. At the age of under 50, however, she should maintain it for two years after the last period.