This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Surgery
Surgery
Hysterectomy
Hysterectomy is the surgical removal of a woman’s uterus.
It is the gynaecologist’s surgery par excellence and is performed for various female pathologies.
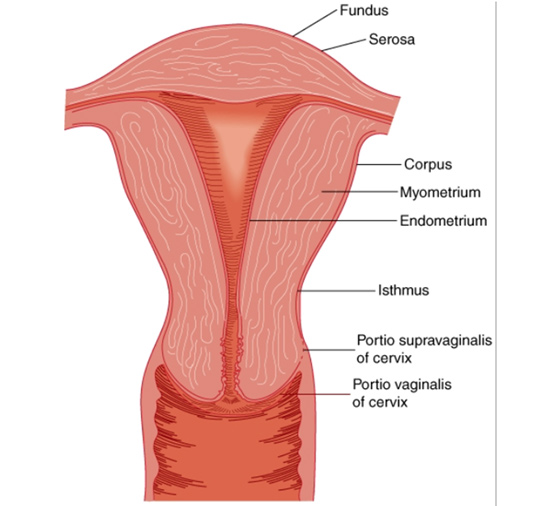
Depending on the type of hysterectomy, we are talking about:
- total (removal of the body of the uterus and the cervix)
- subtotal (removal of the body and preservation of the cervix)
- with the adnexa or without (if we remove the ovaries at the same time or not)
- radical (more extended and specialized surgery that mainly concerns cervical malignancies)
Thus, the types of hysterectomy are adapted to each pathology for which the treating gynecologist indicates an indication for surgery.
Indications may be:
- vaginal bleeding (adenomyosis, fibroids, malignancy)
- pelvic pain (adenomyosis, fibroids)
- prolapse of the uterus (relaxation of the tissues)
- malignancies of the reproductive system (cervical cancer, uterine cancer, fallopian tube cancer, ovarian cancer)
After the operation, with the appropriate painkillers for the first few days, the pain is completely manageable and does not hinder the patient’s daily life. The method with which the operation was performed also contributes to this (eg with laparoscopy the pain is negligible compared to the open method).
Something that worries and is often an inhibiting factor in a woman’s decision to undergo surgery is the fear of her later sex life.
It must be clarified that hysterectomy as an operation does not affect sexual activity, after of course the necessary post-operative period of healing of the internal wound has passed.
Also, the preservation or not of the cervix does not play a role in sexual activity, either for herself or for her partner. On the contrary, the woman freed from the problems that plagued her before the surgery, can now live a normal sex life.
Types of hysterectomy
Hysterectomy can be done with three different methods, under general anesthesia.
- The classic “open” method where we operate with a transverse incision (like a caesarean section) just above the pubic bone.
- The vaginal method, where the removal of the uterus is done entirely through the natural path (vaginal), without an obvious incision.
- Laparoscopy, with which the operation is performed through four holes (5 millimeters each) in the abdomen.
Each method is applied according to the underlying pathology in consultation with the wishes of the patient.
In general, when the uterus has very large dimensions, we apply the open method, while wherever possible, we prefer the laparoscopic method, since it offers an almost painless and very quick recovery with very good aesthetic results. In addition, with laparoscopic hysterectomy, we can see and examine the entire abdomen and perform a total hysterectomy (removal of the cervix and uterus), a partial hysterectomy (subtotal hysterectomy, i.e. preservation of the cervix) as well as intervene in other parts of the abdomen if necessary. , such as the fallopian tubes and ovaries or even the appendix.
Vaginal hysterectomy shows excellent postoperative results but lags behind the fact that with this method we do not control the abdomen during the operation and furthermore it is not performed in cases of malignancy.
Blood after hysterectomy
After a hysterectomy, regardless of the method, if the cervix is also removed (total hysterectomy), the vagina is sutured with sutures that absorb on their own after several days. During this time, internal healing has taken place and there is no risk of the wound opening.
In general, we recommend abstinence from sexual intercourse for 6-8 weeks after surgery.
In some cases, however, due to local infection or due to premature intercourse, the stitches may open and bleeding from the vagina may occur. It is usually of little intensity, but in any case it needs an assessment by the treating gynecologist.
In the first days after the operation, however, the presence of blood is normal since it is waste that is expelled from the body and there is no reason for concern.
Swelling after hysterectomy
Swelling after a hysterectomy may occur and last for a few days. It is usually due to the fact that the intestines due to the operation have not returned to their normal function, with the result that gases and feces accumulate inside and cause a feeling of heaviness and swelling. It is more common in case of open surgery and much less if not at all in case of laparoscopic hysterectomy or vaginal hysterectomy. Usually after 2-3 days the intestine starts to “work” and the swelling goes away.
The laparoscopic and vaginal method contributes to the quick recovery of the swelling, since the patient is mobilized much faster after the operation due to the reduced post-operative pain. If the bowel does not “work” after 3 days, then there is a risk of ileus and the situation should be assessed by the attending gynecologist.
In some cases of laparoscopic hysterectomy, abdominal swelling and shoulder pain may occur, which are due to the carbon dioxide that is present in the abdomen after the operation. It is an innocent symptom that subsides after 24-48 hours, when the carbon dioxide is absorbed by the body.